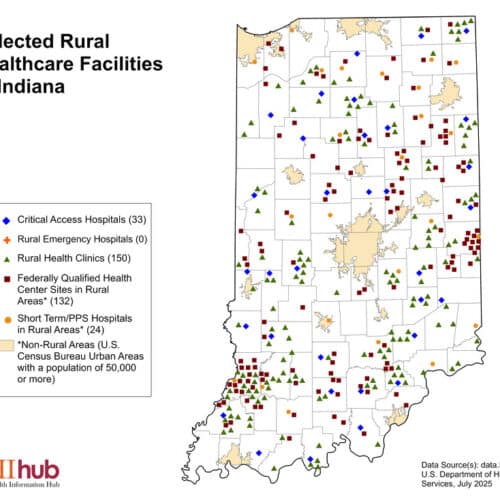
On November 2nd, the Centers for Medicare and Medicaid Services (CMS) issued the CY 2024 Medicare Physician Fee Schedule (MPFS) Final Rule and the CY 2024 Medicare Outpatient Prospective Payment System (OPPS) Final Rule, finalizing several Rural Health Clinic (RHC) specific policy proposals
Intensive Outpatient Program (IOP) Services
• New behavioral health treatment category billable in RHCs beginning January 1, 2024
• Intended for patients with an acute mental illness (including depression, schizophrenia, substance use disorders, etc.) that need between 9-19 hours of care per week
o Higher level of care than occasional outpatient visit; less intensive that partial hospitalization programs
o These services are to be provided in person
• Reimburses through a “special payment rule,” not the AIR/encounter rate
o $284.00 per patient per day
o Reimbursement corresponds to 3* distinct, qualifying services per day
o Costs associated with IOP services must be carved out of RHC cost report
• An IOP service and a separate mental health encounter would not be eligible for same day billing (RHC All Inclusive Rate reimbursement plus $284). However, RHCs could bill for IOP services and a separate medical visit for the same patient on the same day when appropriate.
Three (or fewer services per day) would accommodate occasional instances when a patient is unable to complete a full day of partial hospitalization program (PHP) or intensive outpatient program (IOP). CMS expects that days with fewer than three services would be very infrequent and intends to monitor the provision of these days among providers and individual patients.
Intensive Outpatient Program Patient Eligibility
• Physician* certifies (initially within 30 days and then at least once every other month) that a patient needs behavioral health services between 9-19 hours per week and:
• Is likely to benefit from these coordinated services more than they would individual sessions of outpatient treatment
• Does not need 24-hour care
• Has a separate support system outside of the IOP
• Has received a mental health diagnosis
• Is not a danger to themselves or others
• Has the cognitive and emotional ability to tolerate the IOP
Congress specified in Consolidated Appropriations Act, CAA,2023 that the certifying provider be a physician (MD or DO); this certifying provider cannot be a psychiatric NP or other mental health professional.
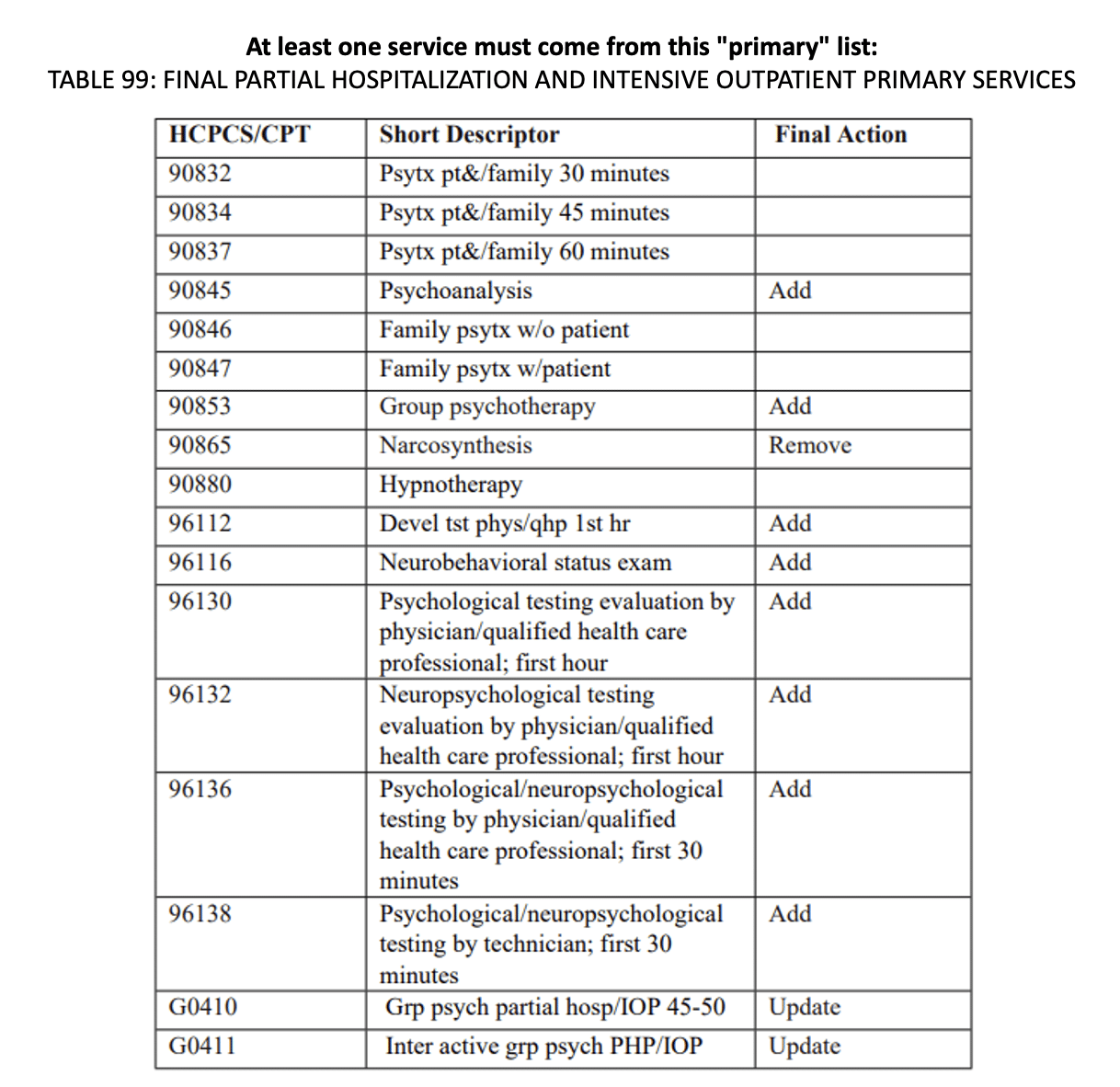
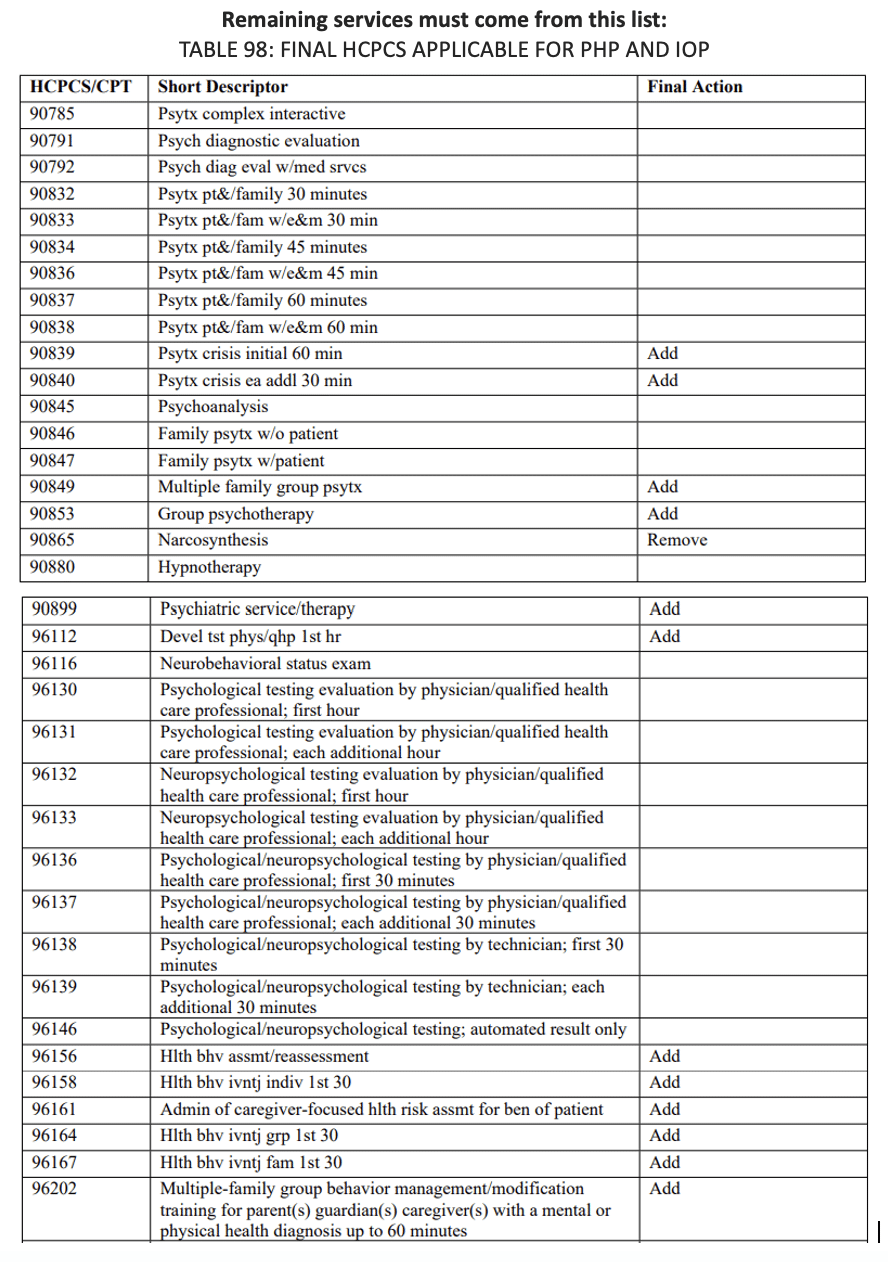
Intensive Outpatient Program Services
• Individual and group therapy with physicians, psychologists, and other mental health professionals as authorized by state law
• Occupational therapy
• Furnishing of drugs and biologics for therapeutic purposes that are not self-administered
• Family counseling (as part of treatment of the patient’s condition)
• Patient training and education
• Individualized activity therapies
• Diagnostic services
• Other related services for diagnosis and active treatment intended to improve or maintain the patient’s condition and function
Please contact Melissa Jones, CRHCP, Rural Health Clinic Senior Associate, Burrows Consulting at melissa@burrowsconsulting.net with any questions.
Written By: Melissa Jones, CRHCP, Rural health Clinic Senior Associate at Burrows Consulting, LLC